Peri-Implantitis & Implant Loss
Monday: 7:30am – 5:00pm
Tuesday: 7:30am – 5:00pm
Wednesday: 7:30am – 5:00pm
Thursday: 7:30am – 5:00pm
Friday: Closed
Peri-Implantitis Complications May Cause Implant Loss
Peri-implant complications can lead to implant loss. Learning to prevent them helps you enjoy your dental implants for a lifetime.
Implants may loosen months or years after being placed. It occurs in only a low percentage of patients. When this happens, an infection called peri-implantitis may develop and be the reason an implant becomes loose or “unseats.”
Dental implants are essentially artificial teeth that replace the root part of natural teeth when missing or failing. They give you a strong foundation for a fixed prosthesis crafted to blend in with your natural teeth. Typically, you can avoid peri-implantitis following your implant placement procedure by adhering to your dentist’s follow-up dental implant care instructions.
What Is Peri-Implantitis?
A patient with peri-implantitis has gum inflammation around a dental implant’s soft tissue and typically has deterioration in the bone supporting the implant. It is a site-specific infectious disease that creates an inflammatory soft tissue issues and bone loss around an osseointegrated implant in function.
According to the bacterial theory, peri-implantitis is best defined as a chronic inflammatory condition associated with a microbial challenge. [1] This definition highlights the need for oral cleanliness and infection control following the procedure.
It is a multi-factorial disease; peri-implant mucositis is classified when inflammation is found only around the soft tissues adjacent to the dental implant, with no evidence of bone loss.
What Causes Peri-Implant Disease?
Established peri-implantitis risk factors include:
- Periodontal disease or possible other medical conditions.
- A lack of proper, at-home implant follow-up maintenance.
- Inadequate long-term patient plaque control.
Any form of cigarette or tobacco use. - Hyperglycaemia.
- Extensive loss of natural dentition.
- The patient struggles with obesity.
- Poorly designed prostheses by an inexperienced dentist.
- The presence of excess cement (poor-quality procedures).
- Inflammation of the mucosa membranes that line the patient’s mouth.
Every individual’s oral health is unique. Your long-term attention to dental care and visits impacts your overall health. This is why making the initial decision to enlist a dental implant service should be carefully assessed by a skilled dentist who knows your history and desired smile design goals.
Peri-Implant Disease Risk
- Indicators
- Red and swelling gums.
- Wobbly dental implant.
- Bleeding gums.
- Signs of infection.
- Decreased jaw bone density.
- Odd breath odor or taste.
By identifying the early signs of peri-implantitis after having a dental implant placement, you gain the most effective treatment.
Let’s look at each indicator more in-depth.
- Red and swelling gums: A key common symptom of peri-implantitis after dental implant placement is redness, swelling, or tenderness near the implant site. This may cause minor discomfort – which is actually a helpful indicator that you should contact your dentist immediately.
- Wobbly dental implant: If the dental implant moves or feels loose, it should be checked out to see whether it is integrating well with your jawbone due to peri-implantitis.
- Bleeding gums: Be observant during your daily oral health cleaning routine to note if your gums are bleeding. This could signal a peri-implantitis issue if it occurs when you are brushing or flossing near your implant area.
- Signs of infection: If a substance, like pus or other infection indicators around the dental implant, is visible, this clearly indicates a potential peri-implantitis issue.
- Decreasing jawbone density: A loss in jawbone density surrounding your dental implant strongly indicates peri-implantitis. A dental implant is deemed successful if there is only 1.5–1.8 mm bone loss during the year after the procedure and not more than 0.2 mm annually.
- Odd breath odor or taste: If someone near you mentions that you have odd or bad breath, note it. There is typically a reason for chronic bad breath – especially after this dental procedure. The same is true if you experience a persistent bad taste in your mouth afterward. It is worth checking out if it’s an indicator of a bacterial infection associated with peri-implantitis.
How To Prevent Peri-Implantitis Disease
Your best prevention method is to be proactive and notice possible signs of complications.
Early diagnosis and prevention of dental implant complications are:
- The most cost-effective tooth implant treatment.
Involve the least amount of pain. - Require fewer trips to the dentist.
Ensure long-term, satisfying results.
The primary way to prevent complications is to avoid bacteria that can colonize around the implant abutment surface. If left untreated, it potentially affects the bone level around the implant.
Can peri-implantitis go away on its own?
How rapidly does peri-implantitis get worse?
Peri-implantitis tissue has extracellular matrix antibodies. The disease progression rate is more rapid and generates a faster and more severe loss of bone compared with periodontal disease. Maintaining overall excellent health will always be a plus and help your body recover. A nonlinear type of progressive bone destruction takes place over time in peri-implantitis.
How rapidly your peri-implantitis worsens depends, in part, on the differences in microorganisms at the implant sites, your body’s defense mechanism, and the absence of a periodontal ligament. A CBCT digital scan helps with diagnosis and treatment.
What does peri-implantitis look like?
As well as the symptoms mentioned above that you may notice, your dentist will look for the following:
- Deepening of the periodontal pockets around the implant.
- Level of exposure and visibility of the underlying implant threads.
- If the implant itself has loosened.
- Any pus discharging from the tissues around the implant.
How is Peri-Implantitis Treated?
Nonsurgical peri-implantitis treatments that commonly resolve issues:
- Mechanical Methods: Mechanical debridement effectively reduces inflammation by removing microbial plaque on the implant surface.
- Antiseptics: Clinically approved antiseptics may be prescribed for reducing bacterial counts. Your dentist may suggest an in-office local irrigation as well.
Antibiotics and - Antimicrobial Agents: Your dentist may prescribe an antibiotic, such as minocycline or doxycycline hyclate, to improve gingival inflammation.
- Plaque control: The management of implant infection starts with a focus on the control of infection.
Peri-implantitis surgical treatments are available. First, we determine an appropriate management strategy, including local and systemic factors. Our dental office provides long-term supportive services and at-home instructions for peri-implant diseases. Our chief goals are infection control, preventing disease progression, and restoring lost bone.
We can restore people with non-ideal functional occlusal issues by reestablishing a functional occlusion with the correct occlusal vertical dimension. Seniors often benefit from restorative dentistry of this type.
Oral laser treatment often provides a short-term decrease in periodontal pocket depth; additionally, air powder abrasives are effective to clean a previously contaminated implant surface. Surgical elimination of a pocket, and bone recontouring are also effective for treating peri-implantitis.
At Woodbury, MN’s Montgomery Dental Care, we ensure a top-level professional process through all procedures and follow-up visits from your first evaluation. Our passion is to offer you the best dentist’s skills, knowledge, modern dental implant technology, and materials available today. The following quote underscores the importance of your specialist’s skill level and experience.
“Bone-level implant designs, combined with convex restorations at an angle exceeding 30°, significantly augment the risk of peri-implantitis.
Nevertheless, a systematic review evaluating earlier systematic analyses favored platform switching for peri-implant bone preservation. This could be due to the relocation of the microgap between the implant and the abutment. This microgap is wide enough to allow for bacterial colonization, and its horizontal offset away from the bone is believed to reduce the risk of peri-implant inflammation. Platform switching has also been supported by a recent clinical study that showed a significantly reduced probability of developing peri-implantitis. – A Comprehensive Review of Peri-implantitis Risk Factors
Dena Hashim’s July 27, 2020 article also suggests platform switching to reduce peri-implant bone loss.
Successful restoration dentistry is always a partnership between you and your dentist. The observant patient who notices any of the above symptoms following an implant placement has the best chance of saving the dental implant.
Peri-Implant Health Can Protect Your Dental Implant
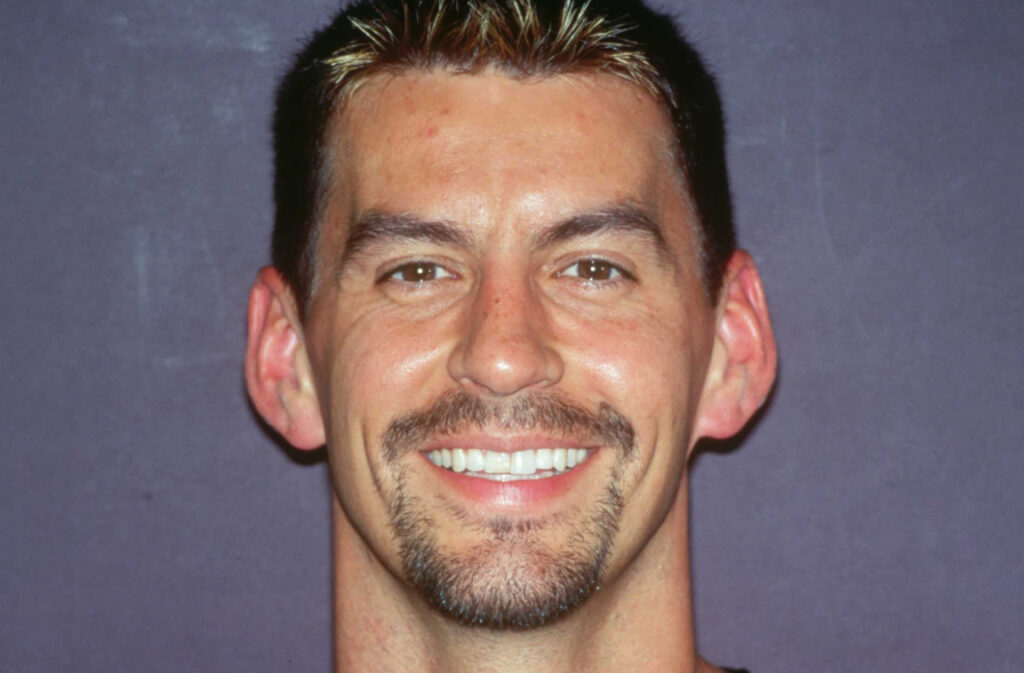
Peri-implantitis is rare. Our patient success rate is exceptional; view our gallery of dental implant cases to see for yourself.
Dr. Marc L. Montgomery trains fellow dentists and helps you learn if peri-implantitis is a concern after getting your dental implants. Call our Woodbury, MN office for a dental implant specialist’s diagnosis to determine if you have peri-implantitis.
Call 651-738-1880
Resources:
[1] Alberto Monje, et al., Understanding Peri-Implantitis as a Plaque-Associated and Site-Specific Entity: On the Local Predisposing Factors, Feb 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6406659/
Look Flawless and Radiant Anywhere You Go!